By: Kathy Ruscitto
 For many years we have lived with the concept that primary care is delivered by an office based physician who treats and coordinates all our care. The wisdom and experience primary care physicians have brought to this practice has been remarkable. Over the last several years environmental pressures have brought about an evolution in the Primary Care model leading to unique new access points for patients.
For many years we have lived with the concept that primary care is delivered by an office based physician who treats and coordinates all our care. The wisdom and experience primary care physicians have brought to this practice has been remarkable. Over the last several years environmental pressures have brought about an evolution in the Primary Care model leading to unique new access points for patients.
Covid added to an existing workforce shortage and many physicians faced burnout from growing demands . From 2005 to 2015 there was an 11% drop in primary care physicians. Recent tracking suggests that decline has continued.
The result is the evolution of a broader model of primary care access ranging from Urgent Care, Retail Clinics to Online Telemedicine consults, and Paramedicine Pilots.
Heather Drake Bianchi, CEO of Drakos Dynamics, a provider of urgent care and family medicine in CNY underscores the importance of accessibility. In a recent interview she emphasized the value of being available when patients need care , outside traditional office hours, aligning with the shifting demands of today’s workforce and lifestyle.
Another essential change, is that many sub specialties are now seen as key or integral to the primary care provider. Integrated primary care considers the input from Pharmacy, Dental, Mental Health, Physical Therapy and Health coaching in an integrated record . These teams, often system based , believe primary care has to include a balanced view across all providers. The blending of all these perspectives across an integrated team allows for better delivery of care in a patient collaborative model.
Dr. Julie Colvin a busy Family Physician and Medical Director of Northeast Family Physicians at St. Joseph’s HHC states,
“Healthcare has to change and evolve, and those options will also give patients and providers more flexibility, and will help the healthcare workforce shortage. We want to make sure that the quality of care in those extended fields is the same as traditional medical care.”
These new access points are exploding using technology, remote access to physicians, and even algorithms that direct care based on AI analysis of patients’ answers to questions.
In many ways these new access points are part of an Integrated Primary Care model. In order for that information to be readily available from any access point, it must be integrated across the medical record, or accessible to providers through the Regional Health Information Organization.
It is not unusual for me to find younger patients using these new access points and not having a primary care physician.
For specialty practices I pose the question, have you adjusted your outreach approaches for patients based on these new access points?
The health care environment continues to evolve utilizing the opportunities from technology, and helping patients find the right care, at the right time, in the right setting.
Kruscitto 1/24
Board member and advisor
Resources
Primary Care in the US, a brief history
Primary Care: Past, Present and Future
https://www.medpagetoday.com/opinion/focusonpolicy/103811
https://www.sjhsyr.org/find-a-service-or-specialty/primary-care


 Expert witness testimony is essential to all medical malpractice legal proceedings. Usually, without a medical expert, plaintiffs cannot proceed to trial, and defendants are usually doomed to an adverse jury verdict. Medical experts are recruited in many ways, even from proprietary companies that offer a diverse variety of experts.
Expert witness testimony is essential to all medical malpractice legal proceedings. Usually, without a medical expert, plaintiffs cannot proceed to trial, and defendants are usually doomed to an adverse jury verdict. Medical experts are recruited in many ways, even from proprietary companies that offer a diverse variety of experts. There’s a new epidemic across America–burnout among healthcare workers. Although the initial focus had been on physicians and nurses, a new study found the burnout problem impacting the entire healthcare workforce–pharmacists, social workers, respiratory therapists, hospital security officers, and staff members of health care and public health organizations.
There’s a new epidemic across America–burnout among healthcare workers. Although the initial focus had been on physicians and nurses, a new study found the burnout problem impacting the entire healthcare workforce–pharmacists, social workers, respiratory therapists, hospital security officers, and staff members of health care and public health organizations.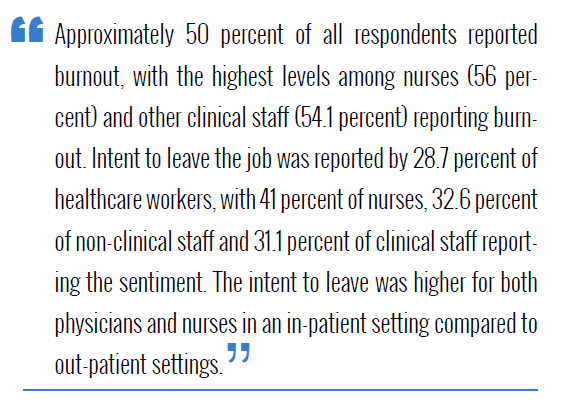
 “We need to increase access to mental health care for health workers. Whether because of a lack of health insurance coverage, insurance networks with too few mental health care providers, or a lack of schedule flexibility for visits, health workers are having a hard time getting mental health care. Expanding the mental health workforce, strengthening the mental health parity laws directed at insurers, and utilizing virtual technology to bring mental health care to workers where they are and on their schedule are essential steps.”
“We need to increase access to mental health care for health workers. Whether because of a lack of health insurance coverage, insurance networks with too few mental health care providers, or a lack of schedule flexibility for visits, health workers are having a hard time getting mental health care. Expanding the mental health workforce, strengthening the mental health parity laws directed at insurers, and utilizing virtual technology to bring mental health care to workers where they are and on their schedule are essential steps.”