By Elizabeth Landry

As the premier bone and joint health provider in the region, OrthoNY aims to provide quality orthopedic care to patients when and where they need it. Formed in 2013 when several smaller, multi-disciplinary orthopedic practices came together to collaborate and build a community practice, OrthoNY encompasses several access points across the region that offer both inpatient and outpatient services. Spanning eight offices, three surgery centers and two orthopedic urgent care locations with a team of 45 physicians, 48 advance practice providers and 16 physical therapists, OrthoNY serves patients from not only the Capital Region and North Country but also from the Hudson Valley to the Canadian border.
With new leadership at the helm, OrthoNY is currently in an exciting period of growth as it expands to continue offering high-quality care to its patient population. Dave Fitzgerald joined OrthoNY in July of 2023 as the new CEO, and he brings with him almost 20 years of experience in physician practice management, specializing in multi-disciplinary, growth-oriented health centers.
For Fitzgerald, his goal in leading OrthoNY comes down to meeting patients’ needs efficiently and effectively, every time. “In orthopedics, it can sometimes be challenging because 100% of our patients are in pain and we’re there to help them through that situation,” he said.
High-Quality Care Through Ambulatory Surgery Centers
From the very beginning of the separate practices that came together to form OrthoNY, a primary driver of expansion has been services offered at outpatient, same-day ambulatory surgery centers, or ASCs. Today, OrthoNY encompasses a total of three surgery centers: Executive Woods Ambulatory Surgery Center (EWASC) and Everett Road Ambulatory Surgery Center (ERASC) in Albany and OrthoNY Surgical Suites (OSS) in Clifton Park. ASCs offer patients efficient, affordable same-day surgery services as opposed to lengthier and often more costly procedures performed in hospital settings.

Created in 1998 and operating as an ASC for almost a decade before OrthoNY was formed, EWASC has seen tremendous success over the years as more and more people have realized the many benefits of one-day surgeries. Kyle Flik, MD, Medical Director for EWASC, compared the patient outcomes at an ambulatory surgery setting versus the surgery process in a hospital setting. “A self-standing surgery center is much more efficient, cost effective and less stressful for patients. We can often provide better outcomes and fewer infections than the alternative hospital setting. It’s a very tight-knit group of people that work together at the ASC every day, which allows us to work smoothly and efficiently as a team. That excellent coordination results in a more condensed experience compared to the time patients would spend at the hospital. In the hospital, a patient of mine might spend 6-8 hours undergoing their operation, but here they would spend 3-4 hours for the same operation and be able to recover in the comfort of their home,” Dr. Flik explained.
 Ellen Cooper, ASC Director at EWASC, explained how the general environment can also lead to higher patient satisfaction. “It’s a very different focus at an ASC,” she said. “If you have your surgery in the hospital, you’ll go to the recovery room and even though you may have had a simple hand surgery or one of Dr. Flik’s knee scopes, you can be placed next to a patient who’s recovering from a major surgery, is on a ventilator and just requires a lot of care. In the ASC, it’s a very different environment altogether. We treat our patients like family and it’s a much more personalized experience.”
Ellen Cooper, ASC Director at EWASC, explained how the general environment can also lead to higher patient satisfaction. “It’s a very different focus at an ASC,” she said. “If you have your surgery in the hospital, you’ll go to the recovery room and even though you may have had a simple hand surgery or one of Dr. Flik’s knee scopes, you can be placed next to a patient who’s recovering from a major surgery, is on a ventilator and just requires a lot of care. In the ASC, it’s a very different environment altogether. We treat our patients like family and it’s a much more personalized experience.”
The surgeons at EWASC typically perform procedures such as shoulder replacements, ACL reconstructions, and hand and foot surgeries, while the physicians at the ERASC location typically perform hip replacements, knee replacements and spinal surgeries. Additionally, the providers at OSS offer sports medicine, pain management, upper and lower total joint replacements, and more. However, all centers offer the same safe, high-quality experience for patients.
Frank Congiusta, MD, President and Medical Director of ERASC and Managing Partner of OrthoNY, pointed out that some patients still have reservations about receiving surgical care at an ASC rather than in the traditional hospital setting. “Some patients are still nervous about getting these surgeries done at surgery centers. I explain to patients that we have the data to prove that in many ways ASCs are safer than the hospital, in terms of lower infection and blood clot rates, because of how quickly we get patients mobilized after surgery and because there aren’t a lot of sick people here. It really is a triple win – we’re able to improve quality while lessening cost and increasing patient satisfaction all at the same time,” he stated.
State-of-the-Art Technology and Innovations
Another aspect of high-quality care offered at OrthoNY’s ASCs is the use of technological advancements that have allowed complex surgeries to move to outpatient settings that were traditionally always performed in hospitals. ERASC has adopted Stryker’s Q Guidance System with Spine Guidance Software, a planning and intraoperative guidance system that enables open or percutaneous computer-assisted spine surgery. This technology allows surgery centers to perform more complex spine surgeries such as lumbar fusions. Robotic-assisted procedures for total and partial joint replacement also help surgeons achieve the desired orientation for the artificial joint through tactile, visual and auditory feedback. Surgeons at ERASC and OSS can perform anterior approach hip replacements, in which the hip joint is accessed without cutting through muscles, leading to decreased pain and higher precision.
Matthew Stein, MD, President

of OSS, explained how these orthopedic innovations bolster the care being offered at OrthoNY. “We feel confident that we are on the front lines of innovation in orthopedic care,” he said. “This includes a growing, evidence-based regenerative medicine program, robotic total joint replacements, minimally invasive, joint preserving surgeries, and an overall transition to outpatient care. We have specialists not only in joint replacement but joint preservation, from cartilage restoration to hip arthroscopy. As a large group with subspeciality training, we have all areas of orthopedics and musculoskeletal care covered.”
One technological advance in outpatient surgeries is the way that anesthesia is used and adapted to allow for patients to return home sooner and also experience lessened pain during recovery. With the increasing interest in outpatient joint replacements, short-acting local anesthetic agents and minimal narcotic use is preferred. This strategy allows patients to be up and moving around within about 45 to 60 minutes of having their joint replaced.
“Some of the cases we’ve evolved are the result of continuing advances in anesthesia. Regional anesthesia has become much more prevalent, and we often use ultrasound-guided local blocks, which can sometimes provide patients with up to twelve hours of pain management that extends well into their recovery at home. These advancements have allowed us to expand the kind of cases we can perform in this environment,” Cooper explained.
Team-Centric Approach Led by Case Management
Perhaps the cornerstone of strong patient outcomes for OrthoNY’s outpatient joint and spine cases, however, is the excellent case management program. Kelly Remancus, ASC Director for ERASC, explained how the current case management program was developed through coordination from the entire staff and physicians. “We have a standardized care map that we follow for all our joint patients. Early on, we brought all our doctors together and discussed how we could standardize the practices we had developed in the hospital setting and implement those same processes for our patients in surgery centers. Using evidence-based medicine, we looked at each aspect of care and decided how we would standardize to provide high-quality care to all our patients,” she said.
At the ASCs within OrthoNY, case management begins as soon as the surgeon and patient decide that the patient is a candidate for ambulatory surgery. The case manager reaches out to the patient, gathers medical records and uses evidence-based screening tools to estimate the patient’s appropriateness for surgery in an outpatient ambulatory setting, as well as identify any conditions that should be optimized or modified before surgery takes place. Once the case manager determines that surgery at an ASC is appropriate, the next initiative is to ensure the patient receives guidance to help prepare for surgery and become educated about every step of the process, accomplished through a patient guidebook and a brief class.
The patient education pathway has also recently been digitized, providing real-time updates and reminders for patients utilizing small digital sound bites via text or email. If a patient needs to start a sanitizing shower four days before surgery, for example, the system will remind the patient five days before surgery, so the reminder is received directly before the preparation needs to be completed. This dynamic education program helps ensure patients accomplish all necessary pre-operative steps, such as getting labs done and attending physical therapy sessions, which helps avoid any delays so surgery can happen on the intended day.

Dawn Allen, Leader of Case Management at OrthoNY, highlighted how the team approach to care helps elevate the case management program and is geared toward maximized patient satisfaction all the way through the process from pre-operative preparation to well after the surgery takes place. “Our team of registered nurses and physical therapists works very closely with other departments, such as preadmission testing, and with the PAs and doctors to make sure the patient is having the best experience. Throughout their journey, we often develop connections with our patients and they appreciate having that clinician support to help guide them. On the day of surgery, there’s usually a case manager on-site at the center for face-to-face support, and we call them a couple days after surgery and then periodically for about 30 days to make sure everything goes smoothly and help work out any issues they encounter. Overall, we receive wonderful feedback from patients and they’re very thankful and happy to have someone to assist them throughout the process,” said Allen.
Continued Growth for the Future
As OrthoNY continues to see high patient satisfaction data stemming from ASC care, it’s clear that expanding offerings at ASCs is the right direction for the future. For Dr. Stein, this growth is one of many aspects contributing to OrthoNY’s leadership in orthopedic care. “I believe the future of OrthoNY is really bright,” he emphasized. “Medicine is constantly changing and orthopedics in no exception. The key is to be a leader in this transition and because of our organizational structure, multidisciplinary approach, regional footprint, and growing outpatient surgery program we are really primed for continued growth. As we have continued to grow, we have brought in experienced administrators to help improve efficiency and quality. We are focused on the optimal patient experience, from the initial appointment all the way through, and believe that as long as we maintain that focus we’ll be ahead of the changes rather than trailing behind.”
 Similarly, according to Fitzgerald, further growing ASC care is a primary goal of OrthoNY moving forward, for the benefit of all at the organization but mostly importantly, for the patients.
Similarly, according to Fitzgerald, further growing ASC care is a primary goal of OrthoNY moving forward, for the benefit of all at the organization but mostly importantly, for the patients.
“There are so many things that excite me about our future,” Fitzgerald said. “Most importantly, we have an incredible clinical and support team in place. My vision is to keep building the practice to support our laser focus on meeting the care needs of our patients. We performed a little over 1,500 total joint replacements in our surgery centers in 2023, and we expect this upward trend to continue in 2024. We want to continue our positive momentum, grow the organization, and do the right service for the right patient in the right place at the right time. I believe this will really solidify us as the top choice for patients in the area.”


 For many years we have lived with the concept that primary care is delivered by an office based physician who treats and coordinates all our care. The wisdom and experience primary care physicians have brought to this practice has been remarkable. Over the last several years environmental pressures have brought about an evolution in the Primary Care model leading to unique new access points for patients.
For many years we have lived with the concept that primary care is delivered by an office based physician who treats and coordinates all our care. The wisdom and experience primary care physicians have brought to this practice has been remarkable. Over the last several years environmental pressures have brought about an evolution in the Primary Care model leading to unique new access points for patients. Expert witness testimony is essential to all medical malpractice legal proceedings. Usually, without a medical expert, plaintiffs cannot proceed to trial, and defendants are usually doomed to an adverse jury verdict. Medical experts are recruited in many ways, even from proprietary companies that offer a diverse variety of experts.
Expert witness testimony is essential to all medical malpractice legal proceedings. Usually, without a medical expert, plaintiffs cannot proceed to trial, and defendants are usually doomed to an adverse jury verdict. Medical experts are recruited in many ways, even from proprietary companies that offer a diverse variety of experts. There’s a new epidemic across America–burnout among healthcare workers. Although the initial focus had been on physicians and nurses, a new study found the burnout problem impacting the entire healthcare workforce–pharmacists, social workers, respiratory therapists, hospital security officers, and staff members of health care and public health organizations.
There’s a new epidemic across America–burnout among healthcare workers. Although the initial focus had been on physicians and nurses, a new study found the burnout problem impacting the entire healthcare workforce–pharmacists, social workers, respiratory therapists, hospital security officers, and staff members of health care and public health organizations.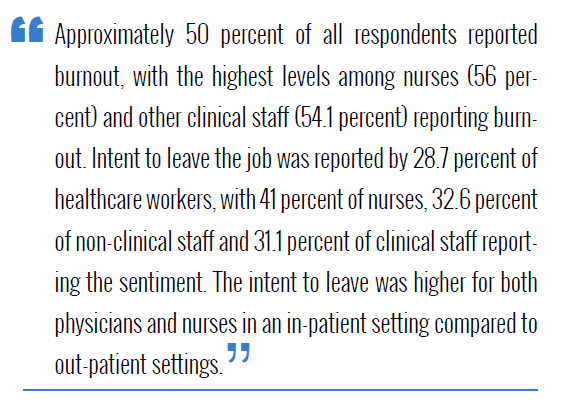
 “We need to increase access to mental health care for health workers. Whether because of a lack of health insurance coverage, insurance networks with too few mental health care providers, or a lack of schedule flexibility for visits, health workers are having a hard time getting mental health care. Expanding the mental health workforce, strengthening the mental health parity laws directed at insurers, and utilizing virtual technology to bring mental health care to workers where they are and on their schedule are essential steps.”
“We need to increase access to mental health care for health workers. Whether because of a lack of health insurance coverage, insurance networks with too few mental health care providers, or a lack of schedule flexibility for visits, health workers are having a hard time getting mental health care. Expanding the mental health workforce, strengthening the mental health parity laws directed at insurers, and utilizing virtual technology to bring mental health care to workers where they are and on their schedule are essential steps.”